Connect With Us
Blog

Risks of Developing Charcot Foot Neuropathy

Charcot foot is a serious condition that develops in people with diabetes, particularly those with peripheral neuropathy, a type of nerve damage that reduces sensation in the feet. This lack of feeling can prevent individuals from noticing injuries, such as small fractures or dislocations, which can worsen over time. As the damage progresses, it can lead to severe foot deformities, chronic ulcers, and in some cases, the need for surgery. Risk factors for Charcot foot neuropathy include long-term diabetes, older age, low bone mineral density, and a history of foot injuries. Early detection and intervention are vital to managing this condition, and a podiatrist plays a critical role in diagnosing and treating Charcot foot. This medically trained foot doctor may suggest custom footwear, casting, and other interventions to prevent further damage and support healing. If you believe you may have foot problems related to neuropathy, it is suggested that you schedule an appointment with a podiatrist for an evaluation and treatment options.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Howard Kimmel, DPM from Buckeye Foot Care. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact one of our offices located in Brook Park and Willoughby, OH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
Are You Suffering From Ingrown Toenails?
Open Reduction and Internal Fixation Surgery for Broken Ankles
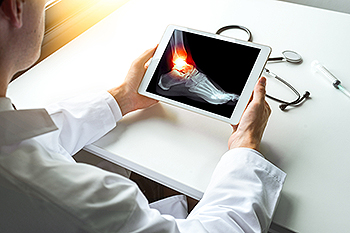
Open reduction and internal fixation, or ORIF, is a surgical procedure used to treat severe ankle fractures. When a bone in the ankle is broken and cannot be realigned through non-surgical methods, ORIF is typically recommended. This procedure involves making an incision over the fracture site to reposition the bone fragments into their correct alignment. Once aligned, the bones are secured with metal plates, screws, or rods to ensure stability and proper healing. ORIF is usually performed when the fracture is displaced, unstable, or involves multiple fragments. It can restore the normal anatomy of the ankle, allowing for proper function and preventing long-term complications such as arthritis. While ORIF is generally successful, it carries risks like any surgery, including infection, nerve damage, blood clots, and complications related to the hardware. If you have sustained a severely broken ankle, it is strongly suggested that you schedule an appointment with a podiatrist to discuss the possibility of ORIF surgery as a treatment worthy of consideration.
Broken ankles need immediate treatment. If you are seeking treatment, contact Howard Kimmel, DPM from Buckeye Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Ankles
A broken ankle is experienced when a person fractures their tibia or fibula in the lower leg and ankle area. Both of these bones are attached at the bottom of the leg and combine to form what we know to be our ankle.
When a physician is referring to a break of the ankle, he or she is usually referring to a break in the area where the tibia and fibula are joined to create our ankle joint. Ankles are more prone to fractures because the ankle is an area that suffers a lot of pressure and stress. There are some obvious signs when a person experiences a fractured ankle, and the following symptoms may be present.
Symptoms of a Fractured Ankle
- Excessive pain when the area is touched or when any pressure is placed on the ankle
- Swelling around the area
- Bruising of the area
- Area appears to be deformed
If you suspect an ankle fracture, it is recommended to seek treatment as soon as possible. The sooner you have your podiatrist diagnose the fracture, the quicker you’ll be on the way towards recovery.
If you have any questions, please feel free to contact one of our offices located in Brook Park and Willoughby, OH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Broken Ankle Causes, Differences, Symptoms and Treatments
The ankle is a hinged synovial joint made up of three bones: the tibia (shin bone), the fibula (outer ankle bone), and the talus (between the heel and leg). These three bones are bound, supported, and stabilized by strong, fibrous bands of tissue called ligaments.
A break in an ankle bone can be either traumatic or stress related. This injury may be referred to as a break or fracture. A traumatic fracture can result from tripping, twisting or rolling the ankle, falling, or by blunt impact to the ankle. These traumatic ankle breaks usually occur during sporting activities or accidents. Stress fractures, however, occur over time and are the result of repetitive stress to the ankle. These fractures sometimes occur when a new activity that engages the ankle is introduced, or when the level of activity is abruptly increased or intensified.
There are various symptoms that accompany an ankle break. The most significant symptoms are pain and swelling that occurs in the ankle and sometimes spreads up from the foot to below the knee. Bruising or discoloration may develop eventually. It will be difficult or even impossible to put weight on the affected foot, and in severe cases there may be a visible deformity or even exposed bone.
It is very important to seek immediate treatment when an ankle break occurs or is suspected to have occurred, in order to allow the bone to properly heal and to avoid future complications such as stiff joints, limited range of motion, and osteoarthritis.
To diagnose a broken ankle, your podiatrist will first ask you to explain how the injury occurred and what your symptoms are. They will perform a thorough examination, checking for damage to nerves, blood vessels, and other structures around the injury site. They will also test your range of motion. An X-ray will need to be reviewed and, in some cases, an MRI or CT scan may be necessary.
Proper treatment of a broken ankle will depend on where and how severe the break is, how stable the ankle is, and whether the bone is displaced (misaligned or separated) or non-displaced (broken yet still aligned properly).
Mild fractures (where the bone is non-displaced) may be treated by resting, icing, and elevating the ankle at first, followed by immobilization with a cast or walking boot. Pain and inflammation may be treated with acetaminophen. More severe or complicated fractures where bones or joints are displaced may require surgery.
Recovery time will also vary, and it may take 4-6 weeks or longer for a broken ankle to heal. Your podiatrist will most likely order progressive X-rays or stress tests to be taken in order to monitor the healing process.
Blisters From Athlete’s Foot

Blisters from athlete’s foot are a common result of fungal infections that affect the feet. Symptoms often include red, itchy, and scaly skin, which can develop into painful blisters filled with fluid. These blisters are typically found between the toes or on the soles of the feet. Risk factors for developing athlete’s foot include wearing damp or tight shoes, having sweaty feet, and walking barefoot in public places like swimming pools or locker rooms. Poor foot hygiene and a weakened immune system can also increase susceptibility. When blisters become infected, they may cause increased pain, swelling, and pus. Relief may be found by keeping the feet clean and dry, using antifungal creams, and avoiding scratching the affected areas to prevent spreading the infection. Blisters from athlete’s foot may form in clusters and can cause pain and discomfort. If you have blisters on your feet, it is suggested that you contact a podiatrist who can successfully treat this condition, in addition to relieving other athlete’s foot symptoms.
Blisters may appear as a single bubble or in a cluster. They can cause a lot of pain and may be filled with pus, blood, or watery serum. If your feet are hurting, contact Howard Kimmel, DPM of Buckeye Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters are often the result of friction. This happens due to the constant rubbing from shoes, which can lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
Symptoms
(Blister symptoms may vary depending on what is causing them)
- Bubble of skin filled with fluid
- Redness
- Moderate to severe pain
- Itching
Prevention & Treatment
In order to prevent blisters, you should be sure to wear comfortable shoes with socks that cushion your feet and absorb sweat. Breaking a blister open may increase your chances of developing an infection. However, if your blister breaks, you should wash the area with soap and water immediately and then apply a bandage to the affected area. If your blisters cause severe pain it is important that you call your podiatrist right away.
If you have any questions, please feel free to contact one of our offices located in Brook Park and Willoughby, OH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters on the Feet
Blisters are a common ailment of people who wear shoes that are either too tight or rub against the feet in an uncomfortable way. Knowing the basics of blisters is important for understanding how they are formed and what treatments should be used for them.
A blister on the foot, or any other part of the body, is a small pocket that is filled with fluid. It usually forms on the upper layer of the skin because these layers are loose enough to allow a blister to form. The most common fluid in a blister is just a clear, watery-like fluid that usually isn’t cause for concern. However, blisters can fill up with blood if they are deep enough and pus if they have become infected with bacteria.
Blisters almost always form on the feet due to shoes rubbing up against the foot, where the friction causes blisters. These can occur after you have walked for a long period of time or when your shoes do not fit you properly. Your feet are also more prone to blisters if they are moist, so keeping them dry and clean is one preventative step you can take.
Preventing infection should be the number one concern when treating blisters, as well as relieving the pain they can cause. Using a bandage to cover up the blister will help it heal and prevent bacteria from entering it. New skin will form under the blister and eventually cause it to pop. You can also take a sterilized pin and try to pop it yourself.
If the blister is filled with pus or blood, seeking treatment from a doctor is ideal. Antibiotics may need to be taken in order to completely eliminate the bacteria inside the blister. See a doctor to have an antibiotic prescribed.
The best way to treat blisters is to prevent them all together. Keeping your feet dry and making sure that your shoes fit properly are just two of the steps you can take to prevent blisters. Shoes that are too tight or shoes that are too loose and allow your feet to slide in them will cause blisters. Applying a bandage to an area where you think a blister is about to form is another way you can prevent them.
Preventing Falls
 Falls are common incidents that can lead to serious injuries, especially in older adults. They occur due to various factors, including poor balance, muscle weakness, vision problems, medication side effects, and environmental hazards like slippery floors or loose rugs. The elderly, particularly those with chronic conditions such as arthritis, osteoporosis, or diabetes, are most at risk. As a result of falls, the feet can suffer fractures, sprains, and bruises, which can significantly impair mobility and independence. Preventing falls involves regular exercise to improve strength and balance, ensuring homes are free of tripping hazards, and wearing supportive footwear. Vision checks and reviewing medications with healthcare providers can also help reduce risks. If a fall occurs, immediate treatment includes rest, compression, and elevation for minor injuries. If you have injured your feet from a fall, it is suggested that you visit a podiatrist for treatment and additional fall prevention tips.
Falls are common incidents that can lead to serious injuries, especially in older adults. They occur due to various factors, including poor balance, muscle weakness, vision problems, medication side effects, and environmental hazards like slippery floors or loose rugs. The elderly, particularly those with chronic conditions such as arthritis, osteoporosis, or diabetes, are most at risk. As a result of falls, the feet can suffer fractures, sprains, and bruises, which can significantly impair mobility and independence. Preventing falls involves regular exercise to improve strength and balance, ensuring homes are free of tripping hazards, and wearing supportive footwear. Vision checks and reviewing medications with healthcare providers can also help reduce risks. If a fall occurs, immediate treatment includes rest, compression, and elevation for minor injuries. If you have injured your feet from a fall, it is suggested that you visit a podiatrist for treatment and additional fall prevention tips.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Howard Kimmel, DPM from Buckeye Foot Care. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact one of our offices located in Brook Park and Willoughby, OH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
Foot Deformities in Women Who Wear High Heels

High heels, while fashionable, can contribute to various foot deformities in women. Prolonged wearing of high heels alters the natural alignment of the foot, leading to conditions like bunions, where the big toe is angled inward towards the smaller toes. Hammertoes may develop, causing the toes to bend abnormally due to pressure and restricted space in narrow shoe designs. Additionally, high heels can worsen existing foot conditions, such as plantar fasciitis, contributing to chronic heel pain and inflammation. Achilles tendon shortening and calf muscle tightening are also common, affecting mobility and increasing the risk of injury. To decrease these risks, women can opt for lower-heeled shoes with adequate arch support and a roomy toe box. Regular stretching exercises and alternating heel heights can help maintain foot flexibility and may help reduce the likelihood of developing painful deformities. If you have developed foot pain as a result of wearing high heels, it is suggested that you schedule an appointment with a podiatrist who can offer effective relief remedies and guide you on more suitable shoes to wear.
High heels have a history of causing foot and ankle problems. If you have any concerns about your feet or ankles, contact Howard Kimmel, DPM from Buckeye Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Effects of High Heels on the Feet
High heels are popular shoes among women because of their many styles and societal appeal. Despite this, high heels can still cause many health problems if worn too frequently.
Which Parts of My Body Will Be Affected by High Heels?
- Ankle Joints
- Achilles Tendon – May shorten and stiffen with prolonged wear
- Balls of the Feet
- Knees – Heels cause the knees to bend constantly, creating stress on them
- Back – They decrease the spine’s ability to absorb shock, which may lead to back pain. The vertebrae of the lower back may compress.
What Kinds of Foot Problems Can Develop from Wearing High Heels?
- Corns
- Calluses
- Hammertoe
- Bunions
- Morton’s Neuroma
- Plantar Fasciitis
How Can I Still Wear High Heels and Maintain Foot Health?
If you want to wear high heeled shoes, make sure that you are not wearing them every day, as this will help prevent long term physical problems. Try wearing thicker heels as opposed to stilettos to distribute weight more evenly across the feet. Always make sure you are wearing the proper shoes for the right occasion, such as sneakers for exercising. If you walk to work, try carrying your heels with you and changing into them once you arrive at work. Adding inserts to your heels can help cushion your feet and absorb shock. Full foot inserts or metatarsal pads are available.
If you have any questions please feel free to contact one of our offices located in Brook Park and Willoughby, OH . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.